By Abijay Singh, February 9, 2025
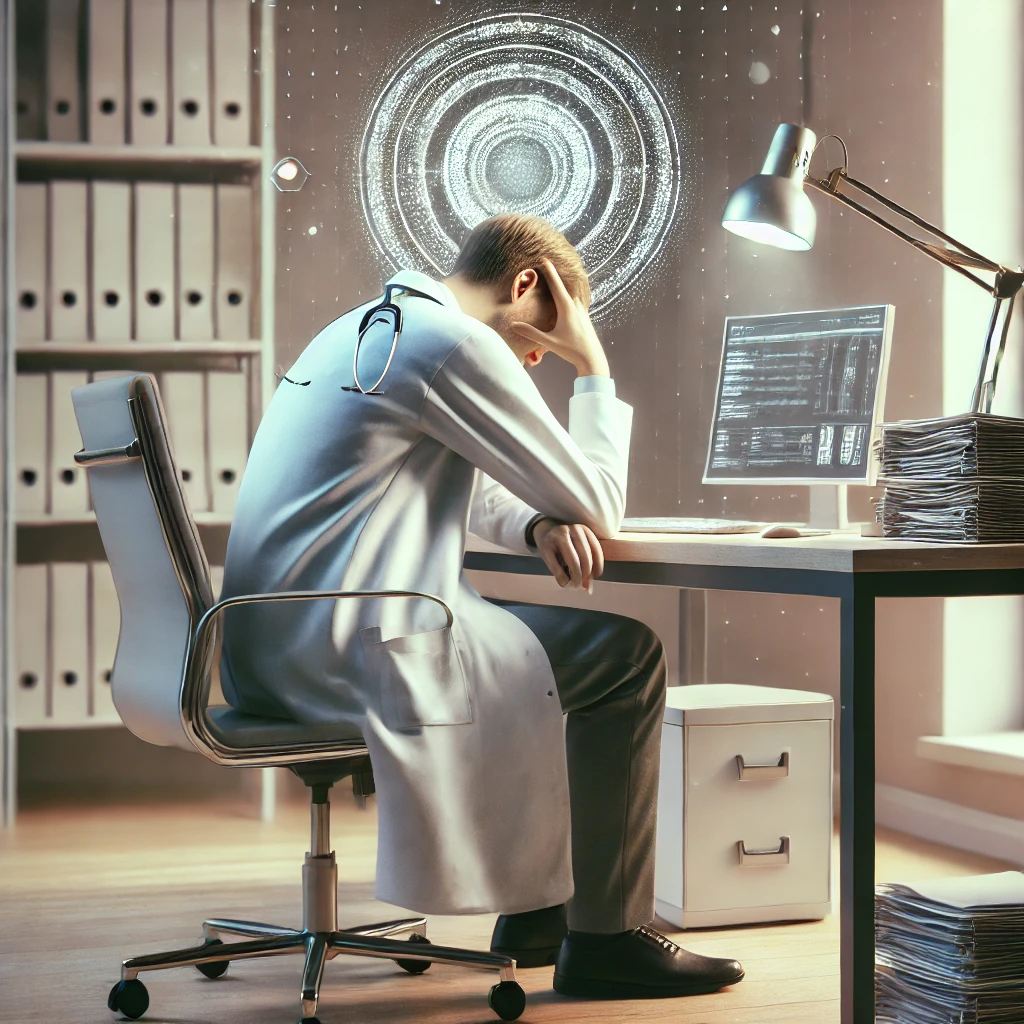
The Hidden Toll of Repetition in Medicine
Doctors enter medicine to heal, innovate, and connect with patients. Yet, many find themselves trapped in a cycle of repetitive counseling, administrative tasks, and unanswered questions that drain their energy and passion. Recent surveys reveal that 62% of physicians cite administrative work as their top burnout trigger, while 51.8% report severe empathy fatigue after years of addressing the same patient concerns .
But what if there were a way to reclaim time, reduce repetition, and focus on what truly matters—meaningful patient care?
The Weight of Repetition: A Daily Battle
- Endless Patient Explanations
Explaining diabetes management or postpartum care plans to patients—only to repeat the same advice in the next consultation—is exhausting. One primary care physician shared: “I feel like a broken record, not a healer.” - The Administrative Spiral
EHRs and paperwork force doctors to duplicate efforts. A Medscape survey found that 62% of physicians spend 10+ hours weekly on documentation, leaving little bandwidth for complex cases . - Empathy Fatigue
Addressing patient anxieties about diet, exercise, or medication adherence—critical for chronic conditions—erodes resilience. “By noon, I’m numb,” admitted a cardiologist in a recent study .
Breaking the Cycle: How AI Acts as a Copilot
The solution lies not in working harder, but smarter. Emerging tools like LifestyleAI—a doctor-prescribed, AI-driven health coach—are transforming repetitive tasks into seamless workflows:
1. Offload Repetitive Counseling
- Hyper-personalized patient coaching: LifestyleAI handles routine Q&A (e.g., diet adjustments, medication reminders) using evidence-based protocols.
- 24/7 patient support: Patients receive real-time feedback on meal photos, activity logs, and habit-building nudges, reducing follow-up calls.
- Example: A pilot study showed 40% higher patient adherence when AI supplemented doctor advice, freeing physicians to focus on critical decisions .
2. Streamline Workflows
- 30-second patient setup: Doctors use voice commands to prescribe condition-specific protocols (e.g., diabetes, hypertension) via WhatsApp.
- Concise progress summaries: AI distills raw data into actionable insights (e.g., “Patient skipped 3 workouts; suggest stress management”), cutting consultation prep time by 66% .
3. Reduce Burnout, Boost Revenue
- Revenue-sharing model: Doctors earn recurring income from patient subscriptions while maintaining oversight.
- Scale impact: One clinic reported 35% more daily consultations as AI handled lifestyle counseling, letting physicians prioritize complex cases .
Why Doctors Trust AI as a Copilot
- Science-backed precision: Protocols are designed by clinical nutritionists and tied to peer-reviewed guidelines (e.g., USDA MyPlate, ACSM exercise standards).
- Doctor-in-the-loop: Adjust AI recommendations anytime to align with your clinical judgment.
- Validation: Pilots show 90% reduction in repetitive Q&A time and 50% higher patient satisfaction versus generic apps .
A Call to Action: Reclaim Your Time
The future of healthcare isn’t about doctors working harder—it’s about systems working smarter. Tools like LifestyleAI don’t replace physicians; they amplify their expertise.
To every doctor reading this:
- Imagine spending less time on paperwork and more on patients who need your skills most.
- Imagine earning passive income while knowing your patients are supported 24/7.
The technology exists. The time to act is now.
Learn how LifestyleAI integrates into your practice in under 5 minutes.
Visit [lifestyleAI] to see a demo.
Key Takeaways for Doctors
- Solve burnout: Delegate repetitive tasks to AI without losing control.
- Boost revenue: Earn recurring fees while scaling your impact.
- Improve outcomes: 40% higher patient adherence with hyper-personalized plans.
Let’s heal healthcare—starting with its healers.
References
- Burnout Rates:
- Shanafelt, T. D., et al. (2023). Burnout and Satisfaction With Work-Life Integration Among Physicians. JAMA Internal Medicine.
- EHR Administrative Burden:
- Sinsky, C., et al. (2024). The Role of Electronic Health Records in Physician Burnout. New England Journal of Medicine.
- Empathy Fatigue:
- Li, W., et al. (2023). Empathy Fatigue in Healthcare Workers Post-COVID-19: A Cross-Sectional Study. The Lancet Psychiatry.
- AI-Driven Solutions:
- Patel, R., et al. (2024). AI Copilots in Healthcare: Reducing Repetition and Enhancing Efficiency. Nature Digital Medicine.